In modern medicine, the mind and body typically stay on two separate tracks. But it’s hard to maintain physical health while suffering from mental conditions.
So Medicaid programs, which insure low-income people, have tried to blend caring for the physical and mental needs of patients, with the hope that it might also save money.
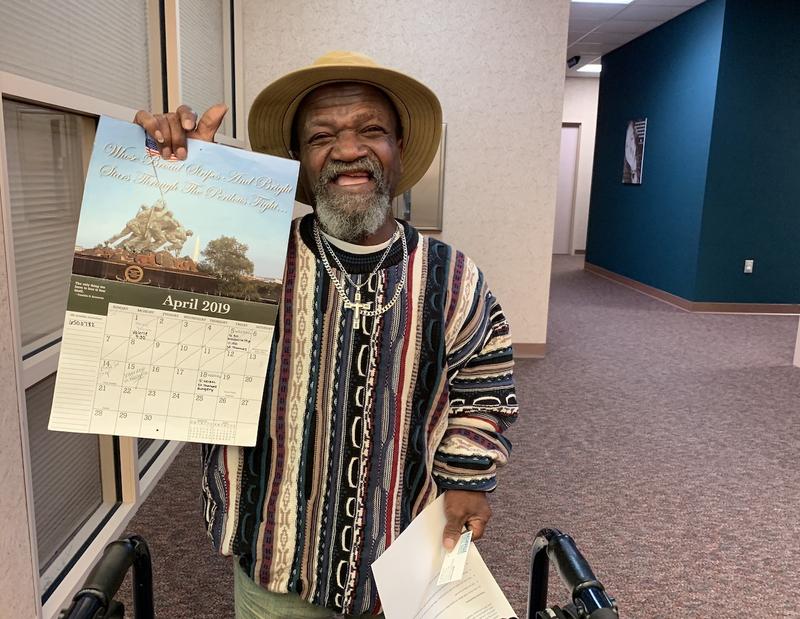
John Poynter of Clarksville has more health problems than he can even recall. “Memory is one of them,” he says with a laugh that punctuates the end of nearly every sentence.
Poynter is currently recovering from his second hip replacement related to his dwarfism. He gets around with a walker covered in keychains from everywhere he’s been. He’s also diabetic and in a constant struggle to moderate his blood sugar.
But most of his challenges revolve around one destructive behavior — drinking.
“I stayed so drunk, I didn’t know what health was,” Poynter says with his trademark chuckle.
His lack of awareness didn’t mean he wasn’t using the health care system. And whether it was a car wreck or a glucose spike, he was going to the emergency room, where everything is more expensive.
The Case For Mind-Body Coordination
Tennessee’s Medicaid program, known as TennCare, has more than 100,000 patients in similar circumstances to Poynter. They’ve had a psychiatric inpatient or stabilization episode along with an official mental health diagnosis.
Their behavioral health condition might be manageable, like addiction or bipolar disorder, but it’s holding back their physical health — or vice versa.
“They’re high-use patients. They’re not necessarily high-need patients,” says Roger Kathol, a psychiatrist and internist who consults with hospitals and health plans trying to integrate mental and physical care.
As studies have shown, these dual-track patients end up consuming way more care than they need, essentially wasting everyone’s time. Kathol says a patient’s hypertension will never be controlled if their mental state keeps them from taking the necessary medication.
“So essentially they don’t get better either behaviorally or medically because their untreated behavioral health illness continues to prevent them from following through on the medical recommendations,” Kathol says.
But coordinating mental and phyical health care presents business challenges because usually two different entities pay the bills, even within Medicaid programs. That’s why TennCare started offering incentives to reward team work.
Health Link
The program, known as Tennessee Health Link, launched in December 2016. The agency paid out nearly $7 million in bonuses the first year. And that’s because studies show the teamwork could end up saving TennCare hundreds of dollars per year, per patient. And a 2018 study from consulting firm Milliman finds most of the savings are on the medical side, not from trimming mental health treatment.
A TennCare spokesperson says it’s too early to say whether the program is improving health or saving money. But already, TennCare is seeing fewer visits to emergency rooms, which is a start.
While there’s a financial case for coordination, it could also save lives. Studies show patients with chronic physical conditions and a mental illness tend to die young.
“They’re not dying from behavioral health,” says Mandi Ryan, director of health care innovation at Centerstone, a multi-state mental health provider. “They’re dying from preventative physical health. So that’s where we really started to focus on how can we look at this whole person.”
But refocusing has required changing the system.
“We don’t really get taught about hypertension and hyperlipidemia,” says Valerie Klein, an integrated care manager at Centerstone. “But when we look at the big picture, we realize that if we’re helping them improve their physical health, even if it’s just making sure they got to their appointments, then we’re helping them improve their emotional health as well.”
Klein, who is based in Centerstone’s Clarksville office, now keeps Poynter on track. Her name appears regularly on a wall calendar where he writes down his appointments. She helped schedule a recent hip surgery and knows his medications better than he does.
Poynter calls Klein “my backbone.”
“I don’t know why we didn’t realize that looking at the whole person made a difference,” Klein says.


