
Life was upended for LaShonia Ingram of Memphis over the last year, and a shadow still follows her around.
Search her name online, and the first result includes the words “fraud” and “most wanted.”
“It was horrible. I couldn’t get a job,” the 42-year-old mother says. “All doors were being closed in my face.”
She resorted to selling purses out of her trunk to support her family. Even DoorDash and Uber wouldn’t allow her to work with a felony charge. The state of Tennessee accused her of illegally living across town in Horn Lake, Miss., while on the state’s Medicaid program, known as TennCare.
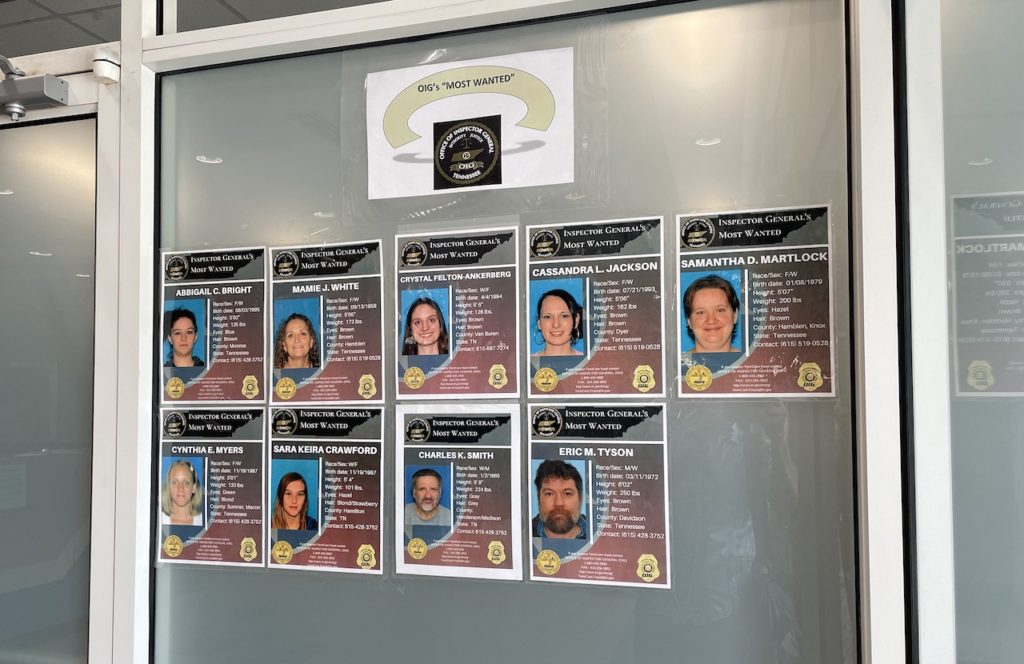
Tennessee is one of the most aggressive states in the nation toward Medicaid fraud among beneficiaries, though it has less and less to show for its efforts. The state posts the names and photos of people arrested for fraud. Some, like Ingram, even wind up on a “most wanted” list, as if they were dangerous and on the run. But increasingly, they’re being arrested for moving out of state — often within the same community — without canceling their benefits.
Ingram was one of 28 Medicaid beneficiaries in Tennessee charged in 2022, according to the Tennessee Office of Inspector General. More than a third of them were accused of not being a Tennessee resident, with many cases originating in Memphis, where some of the suburbs are in Mississippi. They’re also from other state-line communities such as Clarksville and Chattanooga.
 Blake Farmer WPLN News
Blake Farmer WPLN NewsTennessee maintains a “most wanted” list of people accused of Medicaid fraud. While most people see them online, these are taped to the wall outside the Tennessee Office of the Inspector General, which investigates the fraud.
In Ingram’s case, Tennessee announced her arrest in a press release, saying she “eluded” authorities for nearly a year. Ingram says she didn’t have a clue about the charges until she got a ticket for not wearing her seatbelt.
“They pulled me over, and they said, ‘You have a felony warrant.’ And I said, ‘Quit lying,’” she recalls. “I’ve never been in trouble a day in my life.”
It took $2,000 to bond out of jail and even more to hire an attorney. Not until months later did prosecutors show her the evidence so she could refute it and clear her name.
During the time she was on Tennessee’s Medicaid program and living in Memphis, she also filed for divorce from her husband who lived on the Mississippi side of the city. She still had their old address in Horn Lake on her license, even though she moved within Memphis city limits while they were separated. After providing her Tennessee lease and electric bills, the Shelby County District Attorney dropped the felony charges.
But the damage was done.
More Americans than ever are getting their health insurance through Medicaid. And for the first time since the start of the pandemic, states are going to be verifying income and addresses over the next year. It’s up to each state to determine who is eligible, and how to police potential fraud in the program.
Every state has an office to investigate Medicaid fraud among doctors and other providers — since that’s usually where more money can be recovered. But fewer crack down on patients with the persistence of Tennessee.
“We try to apply the law compassionately,” says Chad Holman, who leads the TennCare OIG.
 Blake Farmer WPLN News
Blake Farmer WPLN NewsChad Holman leads the Tennessee Office Inspector General, which is charged with policing Medicaid fraud, solely among beneficiaries. The office started in 2005 prosecuting drug crimes related to Medicaid but is now charging more people with moving out of state and not canceling their benefits.
Other states have similar units, but don’t name the accused publicly. South Carolina keeps the person’s name anonymous even after they’ve agreed to reimburse the state.
Holman defends Tennessee’s practice of posting a “most wanted” list. He says it’s supposed to be a deterrent.
“It’s not to blast anyone or defame anyone. It’s to simply take care of the business that’s at hand, hold people accountable and do what we’re here to do,” he says.
There used to be many more arrests for far more serious charges, Holman says. Early on, more people on TennCare were using their government benefits to acquire and sell prescription painkillers, which is much harder to do at this point because of new federal regulations.
Now, more of that enforcement is focused on residency. In Memphis, 20 of the 27 Medicaid fraud cases since 2019 were questions of state residency, according to the Shelby County District Attorney. And prosecutors have dropped at least a half dozen cases because the evidence was so weak.
Holman says his office won’t overlook low-level offenses.
“This is not murder,” he says. “But the legislature classified it as a felony, and that’s the law that I’m here to enforce.”
Millions spent on a dwindling caseload
Enforcement is expensive. Holman acknowledges it costs far more to run the TennCare fraud unit than the office will ever recoup from people with limited ability to pay. Even if the state recovered every dollar from charges in 2022, it would be less than $900,000. The office has a budget of $6.4 million a year. Since its creation in 2005, it’s brought in less than $10 million, according to its own press releases, while charging nearly 3,200 people with fraud.
The state offers cash for tips that lead to a conviction, though, in many years, there are none, according to an annual report to the Tennessee legislature. And the rate of arrests has slowed dramatically. It now arrests fewer people in a year than previously it did in a single month.
Michele Johnson, executive director of the Tennessee Justice Center, says policing fraud among TennCare beneficiaries takes time and money that could be spent on something more helpful.
“It’d be great if our leaders would get out of the gotcha game and get into the getting people healthy game,” she says.
Especially now, as Medicaid programs are restarting checks on eligibility, Johnson says recipients shouldn’t have to worry that a mistake could eventually get them arrested.
For LaShonia Ingram in Memphis, she’s bouncing back. She still has legal bills to pay and has grown more frustrated at being ensnared by the state’s Medicaid dragnet.
“They made a big mistake,” she says.

