Tennessee’s Medicaid program, TennCare, has a unit dedicated to rooting out potential fraud among beneficiaries and caregivers. A WPLN story from February showed that while costing taxpayers $6.4 million each year, they recoup far less than that.
Despite these findings, lawmakers renewed TennCare’s Office of the Inspector General when they passed the state’s $56 billion budget last month.
Lola Potter, a spokeswoman for the state Department of Finance and Administration, confirmed the unit’s budget and said they recover funds when possible. She said that people on Medicaid “by definition not wealthy,” so they pay TennCare back slowly.
According to its own press releases, since its creation in 2005, the fraud unit has brought in less than $10 million, while charging nearly 3,200 people. In 2022, only 28 people were charged, with over a third of those related to residency issues.
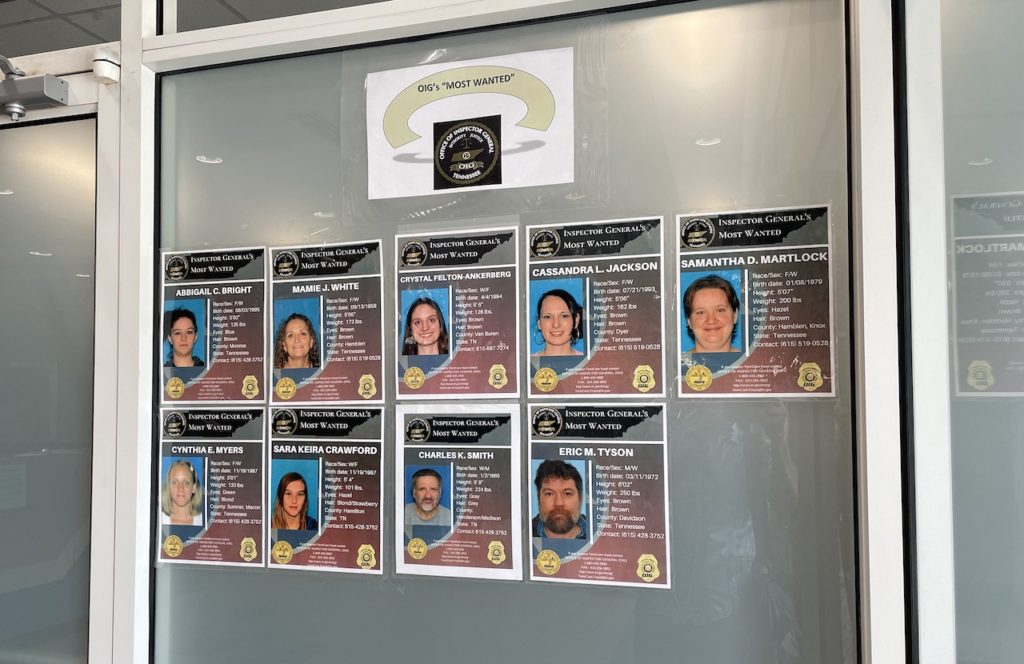
The unit has also raised concerns for its aggressive tactics, such as publicly naming the accused online and putting their faces on a “most wanted” list. One woman in Memphis was charged with a felony and arrested, only later to have the charges dismissed when she verified her residence.
WPLN reached out to lawmakers who approved this year’s budget with the funding. Several declined to comment or said they didn’t know enough about TennCare’s fraud investigations.
One lawmaker, on background, told WPLN that it’s “shocking” that they spend so much to get back so little.
“It’s the price we pay for providing for people who need and deserve assistance,” said Potter.

