Tennessee’s rural hospitals are contemplating a new way to get paid in an effort to stave off their demise. Until now, there have been few solutions put forward — other than having the state expand TennCare to include the working poor, which is unlikely. The latest idea asks insurance companies to prop up rural hospitals, even as they treat fewer patients.
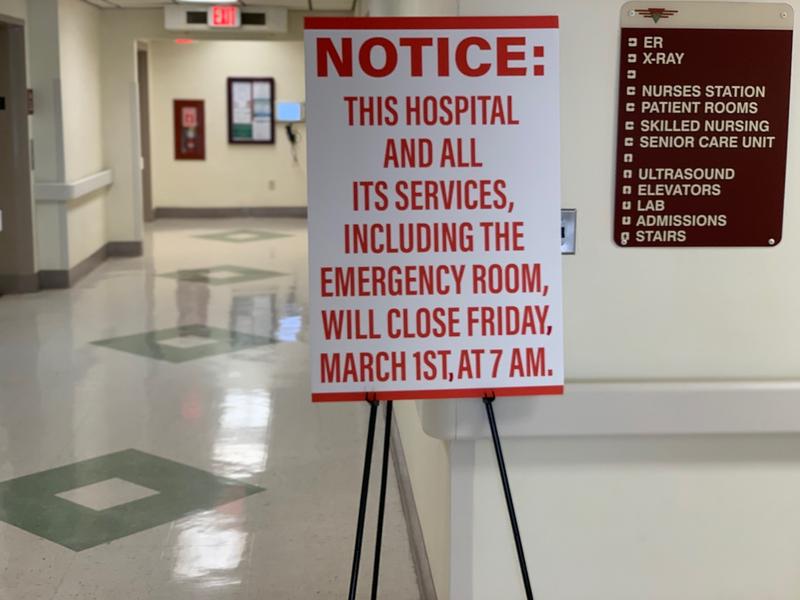
Tennessee has lost 11 rural hospitals (
most recently in Celina), more than any state but Texas. And a recent
consultant’s report by Navigant found at least seven more won’t survive if their financial situation doesn’t improve.
That’s part of the reason Janice Walters came to talk to Tennessee’s rural hospital executives about what they’re trying in Pennsylvania.
“You keep the access, you keep the jobs, which is fundamental to keeping rural America alive,” says Walters, who is chief operating officer of the
PA Rural Health Model. “If we don’t do something, we won’t have rural America.”
More:
Struggling PA Hospitals To Test New Funding Model
Walters says outlying hospitals are more than health care providers. They’re also usually one of the biggest employers in town. But as rural communities continue to shrink, they reach a point where it may not make sense to stay open.
“I mean, you just need people in order to keep a hospital open under the current fee-for-service volume,” Walters says.
And yet just because fewer patients are showing up doesn’t mean a community has no need for its own hospital.
In Pennsylvania, the state’s Department of Health has convinced big insurance companies, Medicare and Medicaid to lock in what they’re currently reimbursing rural hospitals and paying them the same amount on a monthly basis for the next five years.
If the hospitals see fewer patients — which is probable — they can still count on that steady income. The upside for the health plans is that hospitals are supposed to spend some of that money on more than caring for sick patients; they also have to promote wellness.
According to
Modern Healthcare, some have hired staff to focus on tobacco cessation and healthy eating. Others have used the guaranteed money to refocus staff: One hospital added a care manager to help divert some patients from the emergency department. Another is developing telehealth access.
Other possibilities include drug treatment or diabetes prevention.
“Normally you wouldn’t have had the money to do that,” Hospital and Health System Association of Pennsylvania CEO Andy Carter told
WITF. “Now you have this fixed pot of resources that allows you to build the program for better mental health care in the community.”
Pennsylvania’s rural health model is just a few months old. It launched with five participating hospitals with hopes to grow to 30 by 2021. But the Tennessee Hospital Association is watching closely.
“With the number of hospitals we’ve had closed, it’s important that we consider new alternative payment models,” says senior vice president Bill Jolley. “Is it the be-all, save-all for these rural communities? I’m not sure it’s the total answer.”
Jolley has also been pushing some remote hospitals to consider
paring back their services to just an emergency room and outpatient clinic. He says it’s difficult to convince even struggling hospitals to cut services. But it also takes a leap of faith for them to take a set amount from insurers.


