Tennessee ranks among the top five states in the nation for Hepatitis B infections, and policy changes in Washington could make it harder to protect newborns from the virus.
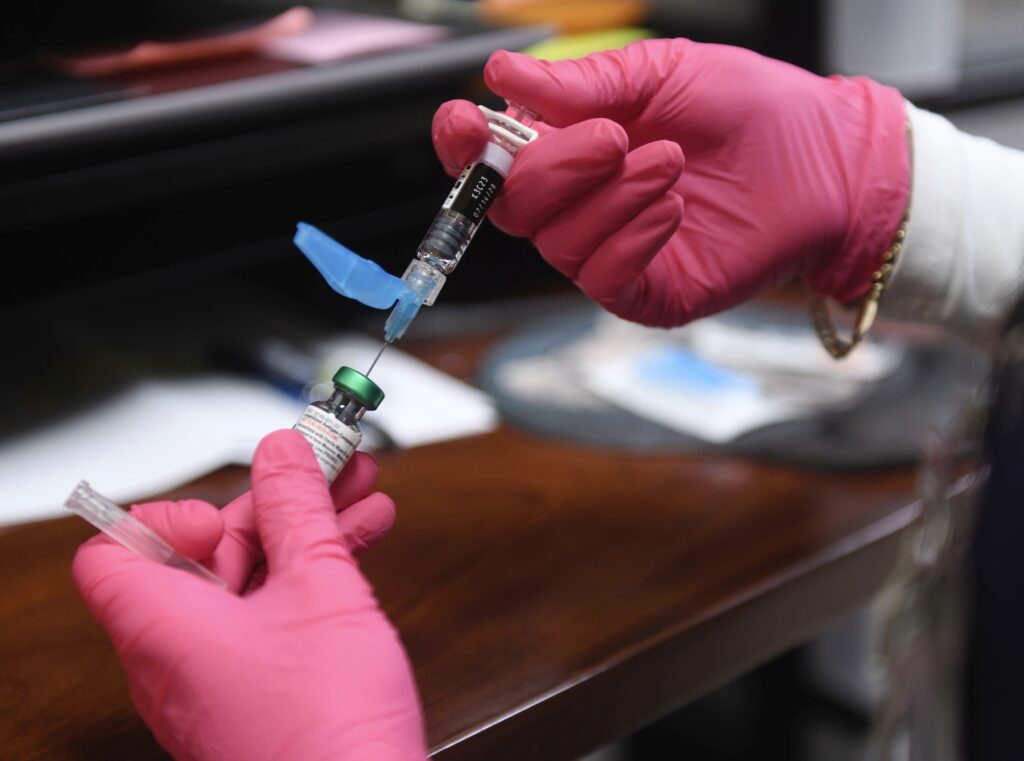
Hepatitis B is especially dangerous for babies. The infection can become a chronic condition that, down the line, can lead to several forms of cancer, liver disease and death. That’s pretty rare for adults who get infected – about 5% of cases. But for infants, that rate is 90%. That’s why it has been standard practice since 1991 to give all infants a Hepatitis B vaccine within 24 hours of birth.
Over several days last week, a federal group called the Advisory Committee on Immunization Practices met in Atlanta. Once a routine if not mundane governing body, the panel has become highly politicized under Health and Human Services Secretary Robert F. Kennedy, Jr. He fired the entirety of the board and replaced them with people who critics call unqualified vaccine opponents.
There was a proposal to loosen the timeline on Hepatitis B vaccines. Under current policy, it’s recommended to be administered within 24 hours of birth.
Hear WPLN’s All Things Consider Host LaTonya Turner discuss this story with Health Reporter Catherine Sweeney in the media player above.
The Hepatitis B discussion came as a surprise because that inoculation hasn’t been as politicized as the MMR vaccine, said Dr. John Heise, a Chattanooga physician who represents Tennessee’s chapter of the American Academy of Pediatrics.
Parents have raised concerns about the MMR vaccine in visits, citing the disproven theory that it causes autism. But, Heise says, he hasn’t heard any parents worried specifically about the Hepatitis B vaccine.
“It’s just more the idea of any vaccines,” he said. “Most of their concern is ‘Do they need to get it done now?’ Because they feel they’re not at high risk as an infant.”
The current recommendation is to get newborns vaccinated immediately. That’s because the virus spreads in blood, and babies can get infected during delivery. Prenatal care often involves testing early in the pregnancy, but it’s not legally required. Parents can get infected while pregnant, and prenatal care isn’t always readily available in Tennessee, as one of every three counties is considered a maternity care desert.
In 2019, 117 babies were born in Tennessee by women infected with Hepatitis B, according to the Centers for Disease Control and Prevention.
For years, Tennessee has ranked among the top five states for new Hepatitis B infections. The state’s infection rate more than doubled from 2006 to 2013, according to a state viral hepatitis report released in 2023. There was a common profile among the people reporting new cases: white people in their 30s who injected drugs.

