The numbers keep climbing in Tennessee, with nearly 2,500 new coronavirus cases confirmed today. That’s a record for the pandemic with more records expected in the coming days.
Health Commissioner Lisa Piercey notes the big increase comes on a day with a record number of tests — nearly 30,000. And she notes the rate of cases turning out positive is still roughly where it’s been for the last few days at roughly 8%.
“The 2,500 number is startling and it’s eye-opening, but it is also in the context of what we’ve been seeing,” she says. “This is not slowing down, but I’m not additionally concerned any more than I was yesterday.”
Beyond the sheer number of positive cases, the state is growing concerned about testing and hospital capacity.
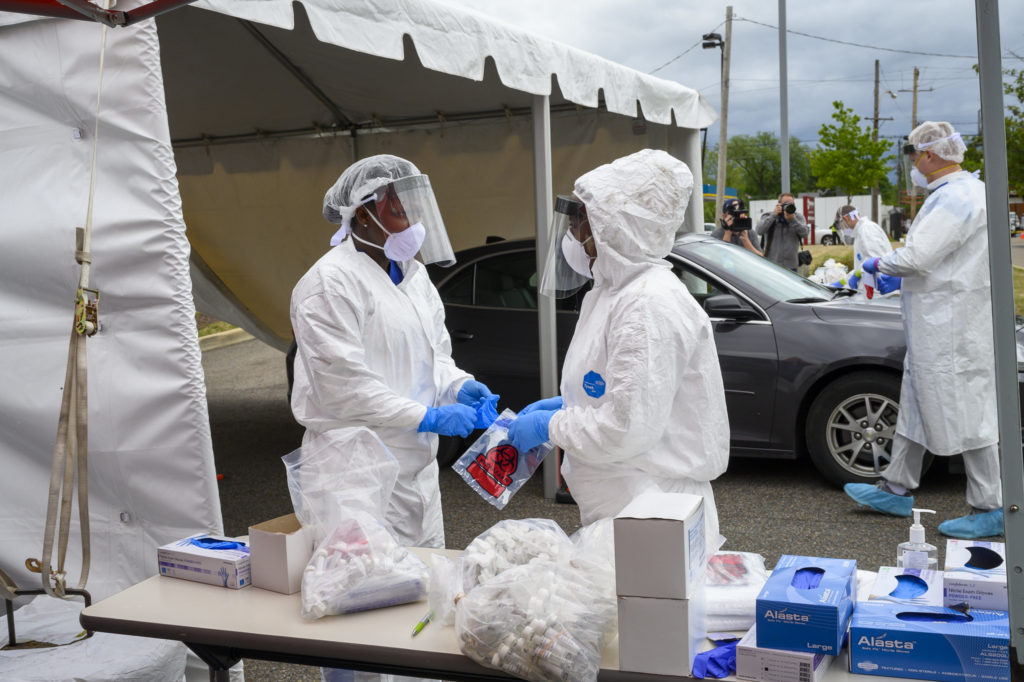
Many states are facing the same challenge. As more people line up for testing, the newly-established systems are being maxed out. Some people, like photographer Kyle Dean Reinford of Inglewood, recently have waited 12 days or more for results.
“That is unacceptable. We can’t get patients back to work, we can’t get contact tracing started until we get that result back in,” Piercey says.
The state, which pays for the bulk of testing, is now diverting samples from backed up labs. They single out Memphis-based AEL, which has been reported to be the biggest source of delays. The Metro Public Health Department in Nashville has recently switched from AEL to Nashville-based PathGroup.
Asked for comment, an AEL spokesperson pointed to a company statement released July 2 warning of delays as the pandemic grows in new regions of the country. AEL also says it’s been prioritizing the “most vulnerable patients.”
But Tennessee health officials disagree with the triage philosophy. They say that means some samples taken from people without symptoms are the most often delayed, or they may never get tested. And they’re the ones most likely to unknowingly spread the coronavirus.
Piercey says asymptomatic testing is key to the state’s strategy. Tennessee was one of the first states to start encouraging everyone to get tested three months ago, no matter the reason.
“Don’t avoid a test just because you are a lower priority from one of these labs,” Piercey says. “It’s still critically important that we have everyone who needs or wants a test to get one.”
Record hospitalizations
Roughly 750 patients statewide are currently hospitalized with COVID-19, a figure that has been rising for weeks. And the state says the cases are becoming more evenly spread out, beyond Memphis and Nashville to Knoxville and Chattanooga, as well as Jackson and the Tri-Cities.
The state hasn’t needed to initiate any of its surge plans. But staffing has become a problem for some hospitals, even when they have the beds available. So the state’s Unified Command Group is beginning to offer assistance when hospitals need help finding doctors and nurses to meet the increasing demand.
But some physicians see a lack of urgency in the state’s response. Nearly 40 critical care doctors spoke out Wednesday.
Dr. Richard Fremont of Meharry Medical College says the capacity issue sneaks up on communities since it usually lags a spike in cases. And COVID-19 patients often stay in the hospital for weeks, especially when they require a ventilator.
“This is why we are seeing shortages in ICU capacity throughout the country where the virus is surging,” Fremont says. “What we in the Tennessee critical care community fear will happen here in our state, if we do not see immediate interventions to reverse the spike in cases.”

