Masks and social distancing are proving to have some major fringe benefits by keeping people from getting all kinds of illnesses — not just COVID-19. But it’s unclear whether the protocols will be worth the pain in the long run.
The teachers at New Hope Academy in Franklin were chatting the other day. The private Christian school has met in person throughout much of the pandemic — requiring masks and trying to keep kids apart, to the degree you can. And Nicole Grayson, who teaches fourth grade, says they realized something peculiar.
“We don’t know anybody that has gotten the flu,” she says. “I don’t know of a student that has gotten strep throat.”
At this point, it’s not just an anecdote.
A study released last week, and led by a Vanderbilt University Medical Center doctor, found that across 44 children’s hospitals, the number of pediatric patients hospitalized for respiratory illnesses is down by 62%. The number of kids in the U.S. who have died from the flu this season remains in the single digits.
Adults aren’t getting sick either. Deaths this season (tracked here) will be measured in the hundreds instead of thousands.
Effective combo
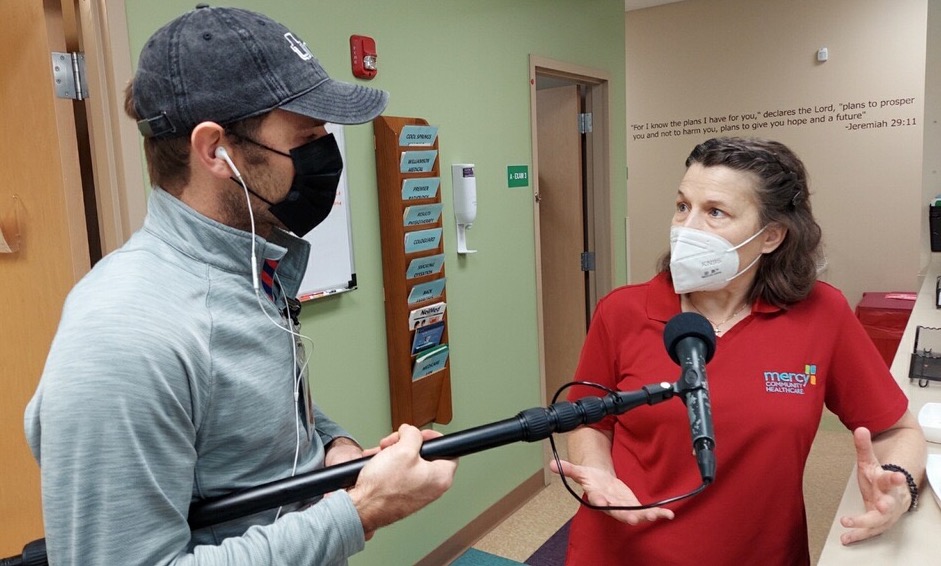
It’s not just the masks and social distance, says Dr. Amy Vehec, a pediatrician at Mercy Community Healthcare in Williamson County. It’s become a serious issue to go anywhere with a fever — so parents don’t send their kids to school, she says.
“They are doing a better job of staying home when they’re sick,” Vehec says. That includes adults who may feel ill.
Isolating when feeling bad could be kept up after the pandemic without too much trouble. But the isolation, the distance and the masks — it’s not working for many kids, Vehec says.
Children with speech trouble aren’t seeing their teacher’s mouth to learn how to speak correctly, for instance.
“I think it has been a necessary evil because of the pandemic, and I have completely supported it, but it has had prices. It’s had consequences,” she says. “Kids’ education is suffering, among other things.”
And with the COVID vaccine not being available to children for a while yet, it may be another year of masks in schools.
For the general public, it’s hard to imagine many people keeping on their masks and giving up handshakes and hugs, says Dr. Ricardo Franco, an infectious disease specialist at the University of Alabama at Birmingham.
“I’m a little skeptical that this crisis will be enough for a wide-spread culture change, given how difficult it’s been to achieve a reasonable culture shift in the previous months,” Franco says.
But the most likely places for permanent change are health care settings.
Dr. Duane Harrison is the medical director for the HCA TriStar emergency department in Hendersonville. It’s a place where even physicians used to get teased for wearing a mask all the time. Harrison says one doctor has donned protective gear since he was hired years ago.
‘Is everyone going to need a break?’
“We used to joke and clown with him about this,” Harrison says.” Until this.”
Now that everyone is in masks, Harrison has found the same thing many other workplaces have — his people aren’t calling out sick, unless it’s COVID.
“When COVID’s done, this is a practice that most of us will probably continue,” he says. “Because we won’t be worried about runny-nose kids or elderly people who don’t know they’re sneezing in your face, and that kind of thing.”
But even believers in the effectiveness of masks have their doubts about the medical community keeping it up.
“The larger question is, is everyone going to need a break?” asks Dr. Joshua Barocas, who specializes in infectious diseases at Boston University.
Either way, public health officials say the time has not yet come to drop mask requirements as we wait for more people to get the COVID vaccine. But eventually, even doctors and nurses are ready to see smiling faces again.
“I know I’m going to need to retire my masks in the future,” Barocas says, “for a little bit.”

